Chronic elevated blood sugar can over time pose serious problems even in those who are not technically diagnosed with diabetes. There have been for instance numerous studies showing that those patients admitted to the hospital who are acutely ill and had higher than normal blood glucose levels were found to have a higher incidence of mortality than those patients with low to normal blood glucose levels. Another study revealed that the mortality rate in those hospitalized patients with hyperglycemia who were not known diabetics was 16% compared to 2% in those who had normal blood sugar levels.
Glycation is a common non-enzymatic process that occurs not only during the cooking process when high heat is used but it also occurs in the human body. In glycation a sugar molecule reacts and bonds with either a fat or protein molecule. Through a subsequent series of slow reactions these molecules can become advanced glycation end products (AGEs). However normal this process is it can reach pathological levels in those with high blood glucose (hyperglycemics and diabetics) which will multiply the production of AGEs. The proteins in the body that commonly react with sugar molecules are found in some of the most delicate tissues of the body including the eyes kidneys arterial and venous structures skin and nerves.
Essentially AGEs are damaged protein complexes and are implicated in many diseases including Alzheimer's cardiovascular disease and cancer. In diabetics their formation is associated with the incidence and progression of diabetic retinopathy nephropathy and neuropathy.
Another protein that is especially vulnerable to glycation is the metalloprotein hemoglobin which of course is responsible for the transport of oxygen from the lungs to the rest of the body. Glycosylated hemoglobin and or HbA1c are the complexes formed in the red blood cell as a product of a glucose/hemoglobin reaction.
A molecule of hemoglobin is made up of four protein chains (two alpha and two beta). Glucose will react and bond to certain positively charged chemical groups located at the start (N-terminal end) of any of these four chains. There is difference however between glycosylated hemoglobin and HbA1c in that glycated hemoglobin is defined as hemoglobin with glucose bound to any of these potential sites. HbA1c is a subset of glycated hemoglobin in that the hemoglobin molecule here binds with glucose bound at the beginning of the beta chain. Generally about half of the glucose is bound to the HbA1c position with the other half bound at three or four other sites.
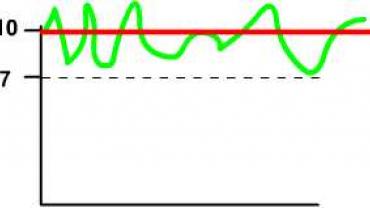
The longer hyperglycemia occurs in blood the more glucose binds to hemoglobin and the higher the level of its glycosylation. And because the life of a red cell averages 120 days the extent that the hemoglobin is glycated can be used as an indication of the average glucose level over the previous one or two months; hence the utility of testing HbA1c in determining medium term glucose levels in those with suspected blood glucose issues or unknown diabetes.
The human genome
An interesting yet complicating factor that may not be appreciated by some practitioners is the fact that glucose metabolism may be greatly predicated upon variations in genetic material. For example the human genome probably evolved in an energy environment in which food was scarce creating a thrifty gene that may be inappropriate in the present day environment of the veritable plentitude of modern day food availability. Add to this the reliance of carbohydrate and processed foods in the modern diet which can activate long term epigenetic changes in the genetic material adversely impacting future progeny. Independent of these factors is another curve ball. HbA1c levels may also be associated with gene variability regardless of variations in genetic glucose metabolism variations and genetic propensities for obesity.
Through the growing science surrounding epigenetics we now know that environmental factors including diet can many times override aberrant genes. Numerous studies for example have shown that making a simple dietary change like reducing carbohydrate intake can positively influence HbA1c generation while also decrease levels of systemic oxidative stress and inflammation.
Unsurprisingly vitamin D as it has been shown to play a key role in many physiological processes appears to have an interesting function in glucose metabolism as vitamin D status has an inverse relation to HbA1c. Repletion of this hormone-like vitamin has been shown to improve HbA1c levels indicating its importance as a possible therapeutic tool.
HbA1c is an important marker that can give valuable insight into the effectiveness of one's therapeutic protocol as well as giving insight into what may be a pre-diabetic state requiring further monitoring as possible proactive intervention.
Michael Fuhrman D.C.