It is well established that sleep is arguably the most important lifestyle factor in supporting and maintaining a healthy physiology. Maintaining a robust and resilient immune system isn’t much different than supporting overall health because it too relies on sufficient sleep. An extensive review published earlier this year explains how “sleep and immunity are bidirectionally linked” - sleep affects both branches of the body’s defense system, and in turn, immune system activation alters sleep. In previous articles, we’ve highlighted how chronic sleep debt is associated with health complications such as metabolic syndrome, obesity, and neurodegenerative disease, as well as how the duration and quality of sleep affect the risk of developing inflammatory bowel diseases.
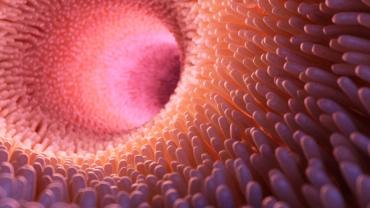
Exciting new research published this month in Science Immunology has identified a unique type of immune cell located in the gut called type 3 innate lymphoid cells (ILC3). These cells are immunomodulatory and sustain equilibrium inside the gut. They are responsible for maintaining proper intestinal function, providing mucosal defense against pathogens, fortifying the gut barrier, and (most recently discovered) keeping track of time! ILC3 cells actively express “clock genes” which are decisive circadian rhythmic genes. Researchers elucidated that these clock genes are particularly active in ILC3 cells and that the production of immune molecules by ILC3 cells adjust to clock gene activity, showing how these genes and intestinal immune cells work harmoniously.
Circadian rhythm (CR) is driven by a molecular clock that influences every single cell in the body and directly affects gut immune function. A healthy gastrointestinal (GI) tract that follows daily rhythms is a prime example of this as ILC3 cells, too, are attuned to CR and play an essential role in that process. Findings from the same animal study showed a correlation between circadian rhythm disturbances and gastrointestinal complications. When researchers genetically modified key clock protein genes in the experimental mice group, they did not produce the intestinal immune cells (ILC3) and subsequently failed to fight off an intestinal bacterial infection, compared to healthy controls. Moreover, the ILC3 cells in the genetically modified mice produced less beneficial T helper cells and more pro-inflammatory immune molecules.
Eating times, gastric motility and emptying, and even gut microbiota are all synchronized with the body’s CR, anticipating the arrival of nutrients into the intestines. A review published in the journal Microorganisms gives evidence that the gut microbial community plays a vital role in promoting proper sleep signals. This research suggests that acute perturbation to the production of clock genes (e.g. erratic sleep patterns, shift work, jet lag, modern-day stressors) directly affects the function of the immune system within the intestines which may help explain the prevalence of inflammatory and autoimmune diseases within the gut. In the aforementioned article, when some mice were put on a schedule similar to a shift worker where the 8-hour light-dark cycle was altered every two days, ILC3 cells no longer operated normally compared to control mice.
Likewise, in another study published in Nature Immunology, researchers identified a molecule called “c-Maf” that is essential for T-helper cells in the gut to develop and function properly. C-Maf prevents the immune system from attacking gut microbiota, therefore if it is missing (e.g. if there is gut dysbiosis) the intestinal immune system will overreact causing a significant shift in the microbial composition. One of the researchers underlines “that both the immune system and the microbiota mutually contribute to establishing and maintaining the balance in the gut” and that “this could explain how a microbial imbalance can contribute to chronic inflammatory bowel disease and why the [conventional] treatment often fails.”
According to another animal study published in May 2019 in Scientific Reports, butyrate - a short-chain fatty acid produced by the bacteria in the large intestine from feeding off of non-digestible fibers - acts as a sleep-inducing signal. When researchers administered butyrate to mice, non-rapid eye movement sleep increased significantly between 50-70% four to six hours after supplementation. This research suggests that butyrate supplementation may be a safe and effective approach for patients who have disrupted sleep cycles and/or who are experiencing gastrointestinal problems.