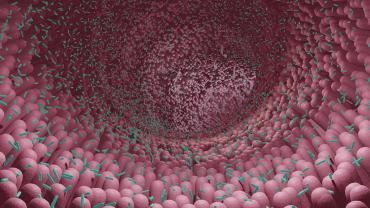
Research demonstrates the role that low-grade inflammation plays in gut microbiome alterations, which can contribute to intestinal barrier dysfunction. Gut barrier health dictates how efficiently micronutrients and water are absorbed. Gut barrier dysfunction (as seen in intestinal permeability) can disrupt nutrient absorption and it increases antigenic exposure with immune activation leading to further intestinal inflammation and gastrointestinal (GI) symptoms.
Serum-derived bovine immunoglobulin/protein isolate (SBI) may support a normal immune response in the gut promoting gut homeostasis.* In animal models of colitis, intestinal inflammatory markers decreased after oral administration of SBI. The SBI contains high concentrations of immunoglobulins with >50% immunoglobulin (Ig)G, 1% IgA, and 5% IgM that can be taken orally. When innate immune cells recognize pathogen-associated molecular patterns (PAMPs), pro-inflammatory mediators and inflammatory pathways, such as nuclear factor-kappa B are activated. Continual PAMP binding may contribute to chronic inflammatory conditions, including inflammatory bowel diseases, irritable bowel syndrome, human immunodeficiency virus (HIV)-related enteropathy, and increased mucosal permeability.
The immunoglobulins in SBI can bind potential endotoxins such as lipopolysaccharides and other pro-inflammatory microbial and viral antigens. Antigens bounds to SBI become much larger molecules, making it more difficult to pass through the epithelium and create an immune response. Fortunately, this binding process does not adversely affect commensal bacteria populations in the gut, further supporting gut microbial health.
Several other studies have shown that SBI may promote mucosal and systemic immune response to infections and reduce markers of GI inflammatory conditions. In a randomized controlled trial, 103 participants receiving suppressive antiretroviral therapy with chronic diarrhea were given either a placebo or SBI (2.5 g or 5 g BID) for 4 weeks, followed by a 20-week placebo-free extension phase with SBI. Markers of GI inflammation were measured by enzyme-linked immunosorbent assay or multiplex assays. After 24 weeks, the results showed SBI significantly decreased circulating intestinal fatty acid–binding protein, zonulin, and interleukin-6, reflecting some improvements in gut barrier function and inflammatory response.
More recent reports note that SBI may even be a promising intervention for novel viral infections by binding and neutralizing pro-inflammatory antigens, decreasing intestinal permeability, and supporting gut microbial health and diversity. In a small, restrospective cohort study, patients with IBD who were considered refractory for standard treatment received 5 g per day of oral SBI for 6 weeks and were assessed GI symptoms before and after treatment. After 6 weeks, patients reported a significant decrease in nausea and diarrhea severity and frequency symptoms.
Along with dietary modifications, such as an elimination diet, low fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAP) diet, and/or anti-inflammatory diet, SBI may help support gut barrier function integrity and intestinal immune health in individuals with functional GI disorders. Unlike bovine colostrum, SBI is dairy-free, so it may be an appropriate alternative to patients with dairy sensitivities or intolerances. However, SBI does contain beef proteins, so those who have an allergy to beef should be cautious. Probiotic and prebiotic supplementation may also support overall gut health and promote beneficial microbial diversity that supports a healthy inflammatory response within the gut.
By Caitlin Higgins, MS, CNS